The rise of powerful weight-loss medications is reshaping health care in the United States, prompting more people to engage with medical services they may have avoided for years, Reuters reports.
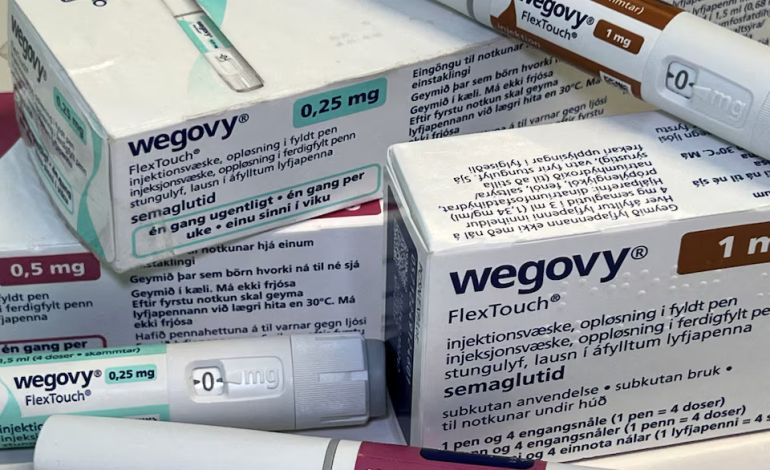
Medications like Wegovy, Ozempic, Mounjaro, and Zepbound — part of a class of drugs known as GLP-1 receptor agonists — are not only helping patients lose significant amounts of weight but also leading to increased diagnoses of obesity-related health conditions.
These drugs are being used to help people lose weight for health reasons, qualify for procedures like fertility treatments or joint replacements, and access long-delayed preventive care. As a result, doctors are seeing more patients with newly diagnosed conditions like sleep apnea, cardiovascular disease, and type 2 diabetes, according to a review of patient health records and interviews with health care professionals.
An analysis of hundreds of thousands of patient health records by the data firm Truveta found measurable increases in the diagnosis of certain obesity-related conditions after patients began using GLP-1 drugs. Between 2020 and 2024, first-time prescriptions for GLP-1 weight-loss drugs increased significantly, and within just 15 days of starting the medication, patients were more likely to be diagnosed with health conditions such as:
- Type 2 diabetes: Diagnoses rose from 32 per 1,000 patients in 2020 to 42 per 1,000 patients in 2024.
- Sleep apnea: Diagnoses increased from 8 per 1,000 patients in 2020 to 11 per 1,000 patients in 2024.
- Cardiovascular disease: Diagnoses grew from 13 per 1,000 patients in 2020 to 15 per 1,000 patients in 2024.
The likelihood of receiving a diagnosis was highest among patients with severe obesity. For example, those with higher body mass indexes (BMIs) were twice as likely to be diagnosed with type 2 diabetes and three times as likely to be diagnosed with sleep apnea compared to patients with lower BMIs.
These increases may seem small on paper, but they signal a broader shift in health care access. The early identification of these conditions could ultimately reduce the need for costlier treatments in the future.
The use of GLP-1 drugs is prompting many patients — especially those who had avoided health care due to the stigma of obesity — to reengage with doctors. According to Dr. Rekha Kumar, a New York-based endocrinologist and obesity specialist, these patients had often felt judged in the past and avoided routine health care as a result.
“This is a population that previously felt stigmatized by health care providers and often didn’t return,” Dr. Kumar explained. “But now that they’re actually seeing themselves get healthier, asking clinicians questions and engaging more, I do think we’re seeing new patients.”
This change is being felt at the front lines of health care. Dr. Courtney Younglove, an obesity medicine specialist and founder of the Heartland Weight Loss clinic in Overland Park, Kansas, said that some patients have been prompted to schedule long-overdue screenings, such as pap smears and colonoscopies. Many of these patients had put off preventative care for years due to the stigma of being overweight.
The story of Phil, a 43-year-old Chicago technology executive, illustrates this trend. He had generally avoided doctors until receiving a GLP-1 prescription from a telehealth provider in 2023. After losing 30 pounds, he felt empowered to ask his doctor for help with other health concerns, such as mental health and addiction issues.
“It gave me the courage to ask,” he said.
For some patients, weight-loss medications offer more than just better health outcomes — they provide access to medical procedures that were previously out of reach. Patients with higher BMIs may be disqualified from certain surgeries, such as joint replacements or organ transplants, until they lose weight. Weight-loss drugs are now helping patients meet the criteria for these life-changing procedures.
At the University of Chicago Medicine, a weight-loss clinic specifically helps patients reduce their BMI to qualify for organ transplants. Before the clinic existed, patients often had no clear path to achieve the weight loss required for surgery, said Anesia Reticker, a clinical pharmacist specialist at the center. Previously, transplant centers might simply tell patients to lose weight on their own, with no additional support or guidance.
The clinic now receives about 100 referrals annually from transplant centers in the Chicago area. Patients like Bensabio Guajardo, a retired steelworker from Indiana, have seen their lives transformed. Guajardo was initially told he was too obese to qualify for a double lung transplant, which he needed due to pulmonary fibrosis. He began taking Ozempic in 2023 and eventually lost 90 pounds, enabling him to undergo surgery. After a successful procedure, his doctors put him back on the drug to help control his blood sugar.
Weight-loss drugs are also being used to help people qualify for joint replacements and fertility treatments. For example, women who want to undergo in vitro fertilization (IVF) may be required to meet specific BMI thresholds before treatment can begin. In some cases, patients are also seeking GLP-1 prescriptions to lower their BMI so they can qualify for knee or hip replacements, which often require a BMI of 40 or below.
“As people’s BMIs come down, they’ll be eligible for surgeries they wouldn’t otherwise,” said Sara Stahl, director of healthcare research at the market analysis firm AlphaSense.
While this trend is still in its early stages, industry experts believe it will become more widespread.
The growing use of GLP-1 weight-loss drugs is expanding the scope of US health care. ResMed, a company that produces sleep apnea devices, attributed its 11% revenue growth in 2023, in part, to increased diagnoses of sleep apnea following the use of GLP-1 drugs.
This influx of newly engaged patients could increase overall health care costs in the short term due to the need for additional tests, screenings, and diagnoses. However, early detection of chronic diseases like type 2 diabetes and cardiovascular disease could lead to lower health care costs over time, according to Andrew Friedson, director of health economics at the Milken Institute.
While the long-term economic impact is still unclear, Friedson sees potential for cost savings.
“The new diagnoses could mean higher initial spending, but early detection could save costs down the line,” he said.
Drugmakers like Novo Nordisk and Eli Lilly have played a central role in developing these GLP-1 weight-loss medications. Both companies have emphasized their commitment to addressing unmet health needs. Novo Nordisk stated that it aims to “address unmet needs for a wider range of patients,” while Eli Lilly underscored the importance of ensuring that adults with obesity have access to diagnosis and evidence-based care.
As demand for GLP-1 drugs continues to rise, their impact on health care is being closely monitored. These medications are encouraging patients to seek care for the first time in years, improving access to critical procedures, and leading to the early detection of serious conditions. Whether the overall effect on health care spending will be positive or negative remains to be seen.
GLP-1 weight-loss drugs are doing more than helping patients shed pounds — they are driving a broader shift in health care. By encouraging patients to seek long-delayed preventive care, qualify for essential surgeries, and address chronic conditions like diabetes, sleep apnea, and cardiovascular disease, these medications are expanding the use of health care services in the US.