A recent study published in the journal JAMA Network Open highlights a significant increase in the use of naloxone, a drug used to reverse opioid overdoses, by non-medical laypersons in the United States, 6 ABC reports.
From June 2020 to June 2022, the number of patients receiving naloxone from bystanders without medical training rose by 43.5%, while emergency medical services (EMS) reported a 6.1% decline in naloxone administration.
The study indicates that these efforts to increase the availability and accessibility of naloxone, commonly known by its brand name Narcan, could be contributing to a broader decline in opioid overdose deaths. The US Centers for Disease Control and Prevention (CDC) reported a 3% decrease in overdose deaths in 2023, marking the first annual decline since 2018.
Chris Gage, the study’s lead author and an EMS Research Fellow with the National Registry of Emergency Medical Technicians, noted the positive implications of this increase.
“The fact that we saw an increase of 43.5% shows that public health efforts are working,” Gage stated.
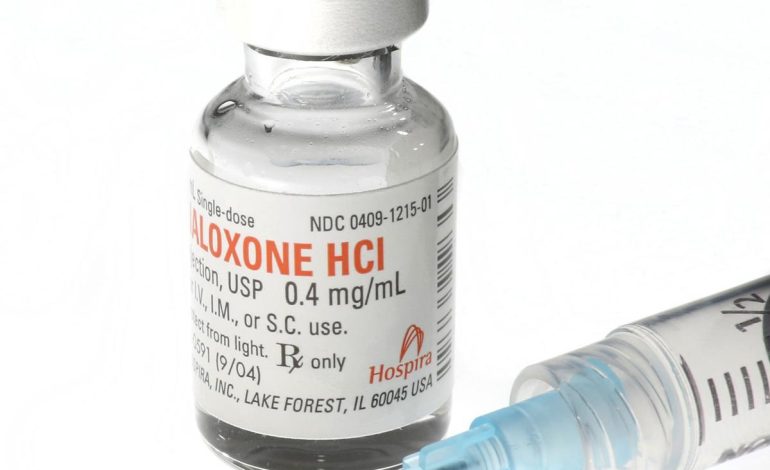
Naloxone is typically administered as a nasal spray and works by reversing the effects of opioids, restoring breathing within two to three minutes. Although it can effectively counteract an overdose, experts advise calling 911 in such situations, as additional medical attention may be necessary.
Gage emphasized the ease of naloxone administration, comparing it to using a nasal spray.
“There’s no real medical training required… Just showing people that they could do something to potentially save someone’s life is the ultimate goal,” he explained.
As naloxone becomes more accessible—recently gaining over-the-counter status with a suggested retail price of around $45 for a two-dose carton—there are still barriers preventing some individuals from obtaining the medication. Dr. Nabarun Dasgupta, a senior scientist at the University of North Carolina at Chapel Hill, highlighted that while the increase in layperson usage is encouraging, further education on drug contamination and access to naloxone is essential.
Despite the rise in layperson-administered naloxone, only 3.4% of the 744,078 naloxone recipients in the study obtained the drug from a bystander. Gage hopes that this percentage will continue to grow, especially as awareness of naloxone’s availability increases.
In conclusion, the study’s findings suggest that increased layperson intervention in opioid overdose situations could play a crucial role in reducing fatalities related to the opioid epidemic.
“If more laypeople are administering naloxone, then hopefully that means these people aren’t dying,” Gage remarked.