A recent increase in pancreatic cancer diagnoses among younger individuals may be less alarming than previously thought, according to a study published in The Annals of Internal Medicine.
While cases among people aged 15 to 39 have surged, researchers found no corresponding rise in deaths, suggesting that the increase may be linked to overdiagnosis rather than a true epidemic.
Initial concern about a spike in pancreatic cancer cases emerged in 2021 when a study led by Dr. Srinivas Gaddam of Cedars-Sinai Medical Center identified a notable rise in diagnoses from 2000 to 2018. Given the often fatal nature of pancreatic cancer, the finding prompted speculation about possible causes, ranging from lifestyle factors like obesity to environmental toxins.
However, the new study, led by Dr. Vishal Patel of Brigham and Women’s Hospital, indicates that the increase has primarily been driven by the detection of early-stage cancers, many of which are unlikely to progress to life-threatening disease. The hallmark of overdiagnosis, researchers say, is a rise in incidence without a corresponding increase in mortality — a pattern evident in the data.
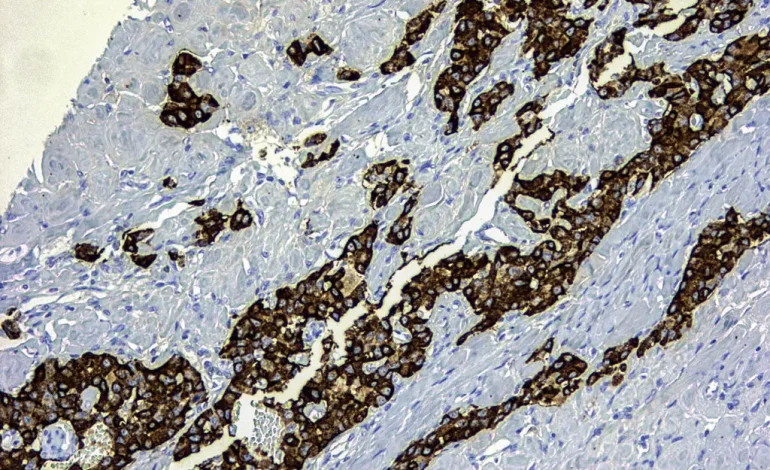
The study highlights an important distinction between two types of pancreatic tumors:
- Adenocarcinomas: These aggressive tumors often remain undetected until they are advanced, leading to symptoms like jaundice and significant weight loss. Notably, the incidence of adenocarcinomas among younger individuals has remained stable over time, indicating no surge in this deadly form of cancer.
- Endocrine Tumors: These slower-growing tumors are less likely to become malignant but are increasingly being identified due to advancements in imaging technology like CT and MRI scans. Many of these tumors would never have caused harm if left undiscovered.
Improved imaging has led to a rise in incidental findings of endocrine tumors during scans conducted for unrelated reasons. While current guidelines recommend monitoring small endocrine tumors, many patients and physicians opt for surgery due to the anxiety associated with a cancer diagnosis. This has led to a doubling of pancreatic surgeries among younger individuals over the study period.
“Surgical intervention has never been proven to be a universally effective strategy for these early-stage tumors,” said Dr. William Jarnagin, a pancreatic cancer specialist.
Yet, the uncertainty about whether these tumors could later become harmful often drives patients to choose aggressive treatment.
The findings have sparked calls to reframe how these tumors are categorized. Labeling all pancreatic tumors as “pancreatic cancer” can create unnecessary fear, leading patients to pursue potentially avoidable treatments. Some experts, including Dr. Arjun Gupta of the University of Minnesota, suggest that separating endocrine tumors from other pancreatic cancers in diagnostic language could help mitigate this issue.
Dr. Gaddam, who initially reported the rise in cases, praised the new study for offering a clearer perspective. He emphasized the importance of explaining the differences between tumor types to patients, noting that this understanding can provide much-needed reassurance.
With input from the New York Times.